Can Concentrated Saline Solution Be Bad for a Baby
Abstract
Hypertonic saline solutions are in broad medicinal apply for treatment of diverse disorders of nose and paranasal sinuses. This trial aimed at the evaluation of safety and efficacy of a hypertonic saline nasal spray within the telescopic of routine care in an otorhinolaryngological outpatient setting. One hundred and thirty-six patients were included into this uncontrolled clinical trial and received 2.7% saline solution nasal spray. Symptoms and clinical signs were documented on an ordinal scale of 0–iv during initial and final examination, and both private symptoms and the sum of symptom scores (clinical sum score) were assessed. Participating patients and physicians furthermore evaluated the clinical benefit of the therapy. Clinical sum score decreased from thirteen.63 ± 6.65 to 7.85 ± half-dozen.79 (p < 0.001) between initial and terminal examination, and significant improvements were observed for ten out of 12 individual symptoms. A clinical benefit was attributed to hypertonic saline treatment by both patients and physicians in more than fifty% of the documented cases. Lxx per centum of the patients noticed improvement of nasal breathing, and l% of the patients considered hypertonic saline an alternative to the use of α-sympathomimetics. One adverse event (epistaxis) was reported, whereas 95% of the patients rated the treatment as flawless. 11 pregnant women and ane nursing mother participated in the trial without the occurrence of any negative effect on mother and child. This written report substantiates the safe and efficacious use of hypertonic saline nasal spray. Reduction in use of classical decongestants constitutes a valuable and safe therapeutic option for patients for whom employ of these drugs is contraindicated.
Clinical Trial Register: DRKS-ID: DRKS00010825
Introduction
Saline nasal applications are broadly used in medicinal therapy. While isotonic saline solutions preferentially aim at cleansing and moistening of the nasal mucosa and thus are suitable for treatment of dry nose symptoms [one], hypertonic saline solutions are rather used for decongestion of the nasal mucosa. With increasing salt concentrations, the pure moistening effect is put in the rear and a water withdrawing effect comes to the fore, leading to decongestion of the afflicted tissues, an activeness particularly wished in cases of viral, bacterial, or allergic rhinosinusitis [2,iii,4,5,half-dozen]. Beyond this osmotic decongesting effect, removal of antigens and inflammatory mediators—thereby reducing the local inflammation—and comeback of mucociliar role may also contribute to relief from symptoms [7]. Dose-dependent agin events due to hypertonicity (e.1000., hurting sensation, nasal blockage, rhinorrhea) accept been demonstrated, occurring commonly when salt concentrations are above approximately 5%. In contrast, therapeutic use of hypertonic saline exhibiting salt concentrations corresponding to less than 3% sodium chloride is generally recommended and well tolerable [8, 9]. Decongestion by apply of hypertonic saline is based on an osmotic effect, leading to the withdrawal of excess liquid from the edematous tissue. This not-pharmacological mode of activeness patently leads to a less fast, less pronounced, and shorter lasting consequence every bit compared to local application of α-sympathomimetic drugs. α-Sympathomimetics mimic the effects of agonists of the sympathetic nervous system on α1 and α2 receptors that lead immediately to constriction of the nasal claret vessels and consequently to nasal decongestion. On the other hand, α-sympathomimetics should not be used for a prolonged time (due to local side effects including rebound reactions and the occurrence of dry nose symptoms) and only after careful hazard–do good assessment in, amongst others, pregnant and lactating women and in patients suffering from cardiovascular diseases. Application of hypertonic saline therefore constitutes an alternative or adjunct treatment to the use of α-sympathomimetic nasal sprays for these populations.
Besides long-continuing apply of big-book saline nasal rinsings that are particularly suitable for cleaning of the nasal mucosa, supporting free nasal animate by softening and dislodging the mucus lining of the nasal cavity, the number of decongesting hypertonic saline nasal spray products increased steadily in the recent years [10]. Notwithstanding, only few data are bachelor on the use of hypertonic saline nasal spray formulations. Nosotros therefore initiated a prospective clinical trial co-ordinate to §23b of the German Medical Device Act in order to assess the clinical benefits of a treatment with a commercially bachelor hypertonic saline nasal spray. No exclusion criteria were prespecified beyond the information given in the Didactics For Use. Clinical investigations co-ordinate to §23b of the High german Medical Device Act are performed with CE-marked, thus marketed, medical devices, must be conducted within the intended apply of the device and without the application of any boosted invasive or otherwise stressful test. By using this blueprint drove of efficacy and safety data in differing indications, periods of treatment and too in special populations such every bit young children, geriatric patients, and pregnant and lactating women were possible inside the scope of routine intendance in an otorhinolaryngological outpatient setting.
Materials and Methods
Trial Design
This clinical trial was based on a prospective, observational, longitudinal design with 2 points of measurement, initial and final exams. The trial was conducted according to §23b of the German Medical Device Act in patients that had an indication for application of hypertonic saline nasal sprays, including merely not limited to, e.g., viral, bacterial, or allergic rhinitis, astute or chronic rhinosinusitis, and use as an alternative to α-sympathomimetics.
The study was carried out in two trial centers in Germany during the catamenia May 2016–August 2017. Patients included in the written report were supposed to be above the historic period of i year or older. No further inclusion or exclusion criteria were defined across the data given in the Educational activity For Use. Nonetheless, the decision to prescribe/recommend hypertonic saline nasal spray to the corresponding patient must have been made by the physician earlier the inclusion of the patient in the trial, and patients were enrolled only subsequently they had been given sufficient information and had provided written consent concerning their participation in the trial. Each patient enrolled was discipline to an initial and a final examination. Due to the non-interventional character of the study, the time grade of the visits was not prespecified.
The trial was performed according to the German Medical Device Deed and the Declaration of Helsinki, was registered in the German Clinical Trial Annals (DRKS-ID: DRKS00010825), and was approved by the Institutional Review Board of the Freiburg Ideals Commission International (Code: 016/1245).
Trial Production
The medical device used in this trial was manufactured at Ursapharm Arzneimittel GmbH, Saarbruecken, Germany. The hypertonic saline nasal spray (hysan® Salinspray) contains two.7% sea salt and purified h2o. Patients were advised to apply the nasal spray several times a 24-hour interval while spraying one to ii sprays into each nostril, in compliance to the manufacturer's Instruction For Use. With each spray, 0.07 mL of saline solution was dispensed. In instance of concomitant handling with other nasal sprays or nasal drops, patients were advised to comply with a time interval of at least thirty min between the applications. In case of the occurrence of hypersensitivity reactions similar itching or redness, patients were advised to discontinue utilise of the product.
Efficacy and Safety Measurements
All information for this written report were recorded on a single case study form (CRF) that was filled in by the dr.. Indications for awarding of hypertonic saline nasal sprays were documented at the initial exam, and symptoms and clinical signs were subsequently documented at both visits (initial and final exam). Impairment of nasal animate/nasal obstruction, sneezing attacks, nasal discharge anterior/runny nose, nasal belch posterior, thick nasal discharge, desire to clear one'southward pharynx/dry throat, redness of nasal mucosa, edema of nasal mucosa, impairment of odour, impairment of taste, impairment of sleep, and impairment of food intake were assessed on an ordinal scale of 0–four (0 = none, 1 = mild, 2 = moderate, 3 = strong, iv = very strong), and the private ratings were documented for each symptom and each visit. Redness of nasal mucosa and edema of nasal mucosa were determined past anterior rhinoscopy; all other parameters assessed were reported past the patients. Scorings of each symptom and clinical sign were summed upwards to the clinical sum score ranging from 0 (no symptoms) to 48 (very strong symptoms). I hundred and xx-nine patients had complete ratings of the clinical sum score at both visits, and missings were not imputed.
In order to evaluate the clinical benefit of the hypertonic saline nasal spray therapy, the physicians involved were too asked to appraise the treatment with the product (very expert–expert–satisfactory–bad), the compliance of the patient (very good–proficient–satisfactory–bad), whether treatment with hypertonic saline should exist continued (yes–no), how they assessed the period until the resumption of activities of daily living equally compared to treatment without hypertonic saline (significantly shorter–shorter–no difference–longer–significantly longer), and whether they would prescribe/recommend the product once more under similar weather condition (yes–no–possibly). During the final exam, the physicians involved likewise evaluated the utilise of α-sympathomimetics by the patients every bit reduced–constant–increased or non assessable.
During the final exam, the patients evaluated the overall treatment event (significantly ameliorate–better–no divergence–worse–significantly worse), their satisfaction with hypertonic saline nasal spray (very skilful–skillful–satisfactory–bad), whether they would utilise it again nether like atmospheric condition (yes–no), when they experienced an comeback of nasal breathing after application of hypertonic saline nasal spray (< 2 min, < 5 min, < 10 min, < 30 min, after repeated application, no improvement), and whether they consider hypertonic saline nasal sprays an culling option for employ of α-sympathomimetics (yes–no–no culling, but adjunct handling).
Tolerability of the product was evaluated by the physicians at the concluding examination using the ratings "flawless," "acceptable," and "non acceptable." Adverse events and severe adverse events had to be documented in the case report form at every visit past the investigator. The occurrence of severe agin events had to be reported to the sponsor of the study within 24 h.
Sample Size and Statistical Analysis
This clinical trial was designed to provide existent-world prove by means of a number of clinically relevant end points. Thus, no primary finish signal for formal sample size adding was defined. According to a pragmatic sample size rationale, the inclusion of a maximum of 150 patients was planned to obtain valid and reliable results regarding safety and efficacy. Patient recruitment took place betwixt May 2016 and August 2017.
Data are presented as hateful (thousand) ± standard deviation (SD) for continuous variables or as relative frequencies (north) and percentages (%) for categorical variables. Occasionally, percentages did not add upwardly to 100% due to rounding. Mann–Whitney U exam was used to compare the interval between initial and final exam between patients with single diagnosis of acute or chronic rhinosinusitis. Clinical sum scores as well equally single symptoms and clinical signs between initial and final examination were compared using Wilcoxon signed-rank tests. Moreover, Kruskal–Wallis H tests were used to compare changes in single symptoms and clinical signs (categorized equally improvement, no change, worsening) for a segment of patients with a clearly divers indication (either astute rhinosinusitis, chronic rhinosinusitis, allergic rhinitis, not-allergic rhinitis, or alternative to apply of α-sympathomimetics, n = 103). A p value of ≤ 0.05 was considered every bit statistically significant. Statistical analyses were explorative. Thus, no adjustments for multiple testing were performed. Normal distribution of metric variables was assessed past Shapiro–Wilk test. All analyses were performed using SAS nine.four (SAS Institute Inc., Cary, NC, USA) and SPSS, version 25 (IBM Germany GmbH, Deutschland).
Results
A total of 136 patients (43 males, 93 females) were included in the report (get-go patient in: May 24, 2016; last patient out: Baronial 7, 2017). Iii patients were lost to follow-upward; thus, the ITT population included n = 136 patients at baseline and due north = 133 at the terminal test. The rubber population comprised all patients included into the report (n = 136) (Fig. 1). On average, the last examination took identify 44.96 (± 51.xiv) days after the initial examination. The time between initial and final test was significantly shorter in patients with acute rhinosinusitis (33.71 ± 38.05 days) than in patients with chronic rhinosinusitis (78.00 ± 98.68 days; U (31,14) = 315, p = 0.016).
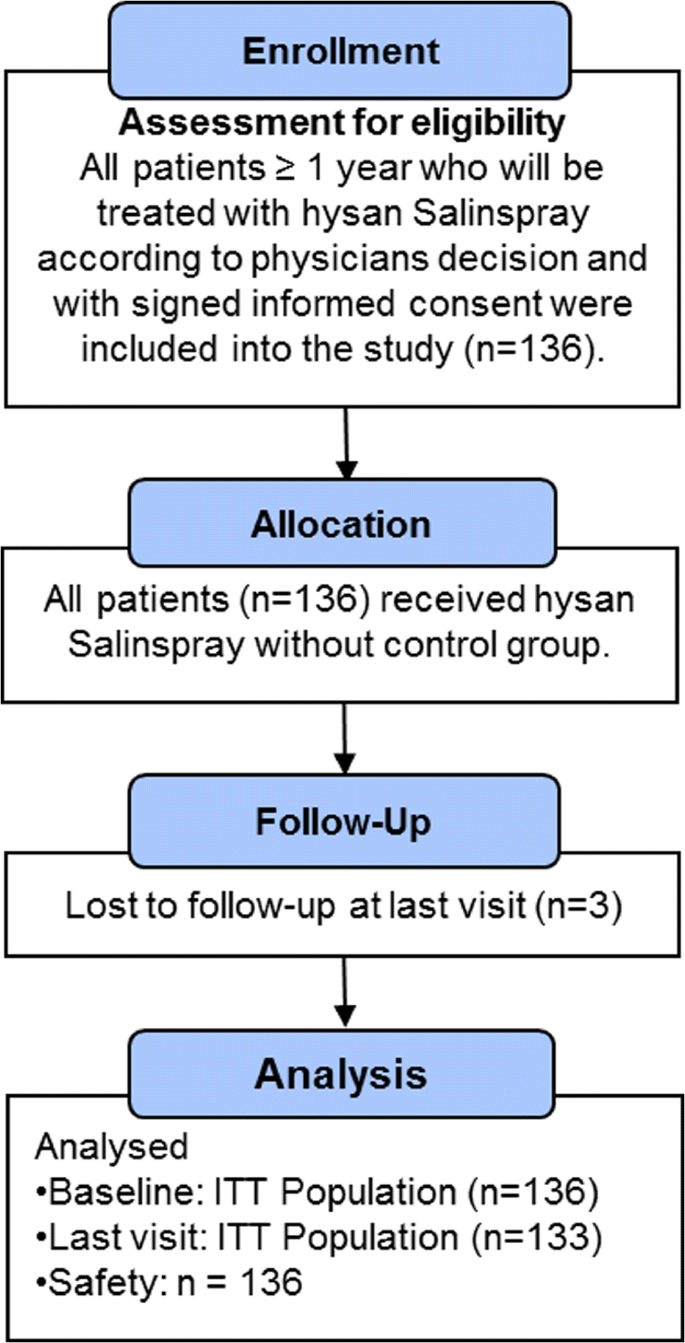
CONSORT flow diagram
Overall, compliance was assessed by the physicians as "very good" in 58%, as "good" in 37%, equally "satisfactory" in 4%, and every bit "bad" in i.5% of the patients.
Demographic data and indications for use of hypertonic saline nasal spray are given in Tables 1 and 2.
Efficacy Stop points
Clinical sum scores (sum of symptom scores for damage of nasal breathing/nasal obstacle, sneezing attacks, nasal belch anterior/runny olfactory organ, nasal belch posterior, thick nasal discharge, desire to articulate ane's throat/dry pharynx, redness of nasal mucosa, edema of nasal mucosa, impairment of odour, impairment of taste, harm of sleep, and impairment of nutrient intake) for the initial and final examinations are given in Fig. 2. Clinical sum score decreased significantly from xiii.63 ± six.65 to 7.85 ± 6.79 score points (z = − 8.06, p < 0.001, n = 129) between initial and terminal exam.
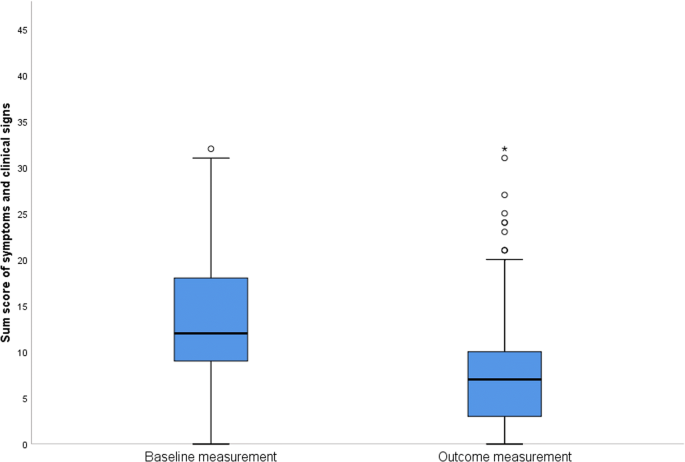
Boxplot of clinical sum scores for initial and terminal examination, representing the sum of symptom scores for damage of nasal breathing/nasal obstacle, sneezing attacks, nasal discharge inductive/runny olfactory organ, nasal discharge posterior, thick nasal discharge, desire to clear one'southward throat/dry throat, redness of nasal mucosa, edema of nasal mucosa, impairment of smell, impairment of taste, impairment of sleep, and impairment of food intake
Ratings for each symptom revealed statistically pregnant reductions in 10 out of 12 symptoms (p < 0.01), but for parameters "damage of gustatory modality" and "damage of food intake" no pregnant change in symptoms was observed (p > 0.05). However, large office of the study population did not express any symptoms already at initial examination for the latter ii parameters (Table 3).
At the final examination, physicians involved assessed the treatment with the product as very good (22%), proficient (35%), satisfactory (35%), or bad (viii%). The treatment should be continued in 42% of the cases (e.g., due to underlying chronical disease); in 58% of the cases, treatment with hypertonic saline was ceased after the final test. Of the physicians, 4.5% assessed the menstruation until the resumption of activities of daily living as compared to a handling without hypertonic saline as significantly shorter, 41% equally shorter; in 53% of the cases, no departure was observed; and in 0.75%, a longer flow was observed. Physicians would prescribe hypertonic saline again in patients with identical diagnoses in 57% of the cases, would non prescribe it in 26%, and would possibly prescribe it in 17% of the cases. Use of α-sympathomimetics was assessed by the physicians as reduced in 34% of the patients, equally abiding in 35%, and as increased in one.5% of the cases. In 29% of the cases, utilise of α-sympathomimetics by the patients was rated as not assessable.
Xiii percent of the patients felt significantly ameliorate during handling, 45% rated their condition equally amend, 38% recognized no divergence, 3% rated their condition as worse, and 0.75% as significantly worse. Satisfaction with hypertonic saline nasal spray was assessed by the patients as very practiced in 16% of the cases, as adept in 38%, as satisfactory in 36%, and as bad in ten% of the cases. Sixty-one percent of the patients would use hypertonic saline nasal spray again under like conditions, and 38% would non.
Fifty percent of the patients considered hypertonic saline nasal sprays every bit an alternative option for use of α-sympathomimetics, whereas xxx% of the patients did non. Fourteen of the patients rated hypertonic saline nasal sprays not as an alternative merely as an adjunct treatment to the use of α-sympathomimetics (6% missing values).
Improvement of nasal breathing after application of hypertonic saline nasal spray was observed in ca. 70% of the patients. Tabular array 4 gives an overview on the onset of improvement as observed by the patients.
In addition, we compared symptoms and clinical signs for specific subgroups of patients. We considered patients who received the hypertonic saline spray for either 1 of the five specific indications: acute rhinosinusitis, chronic rhinosinusitis, allergic rhinitis, not-allergic rhinitis, and alternative to utilize of α-sympathomimetics (n = 103); patients with double indications or "other indications" were omitted from these analyses (n = 33). No significant differences in changes in unmarried symptoms and clinical signs between these specific patient groups were observed for 11 out of 12 parameters tested. A significant departure was establish for parameter "nasal discharge, posterior" (p = 0.011). Patients suffering from "chronic rhinosinusits" were more likely to bear witness improvements (71% comeback vs. 21% no alter vs. 7% worsening) in parameter "nasal discharge, posterior" as compared to patients suffering from "acute rhinosinusitis" (29% improvement, 65% no change, 6% worsening) and using the nasal spray as "alternative to apply of α-sympathomimetics" (fifteen% improvement, 64% no change, 21% worsening).
Safety Evaluation
Tolerability was assessed as "flawless" in 95% of the patients and as "acceptable" in v% of the applications. One patient reported twice about the occurrence of an epistaxis, which was assessed by the physician as being "mayhap related" to the application of the nasal spray.
Xi patients were pregnant during application of the hypertonic saline nasal spray, and one patient was breastfeeding. In none of these patients, any adverse events were reported. Follow-upwards of the pregnancy, thus monitoring of the health status of the newborn, was conducted in ten cases (one case lost to follow-upwards; follow-up during ongoing visits or via telephone). Health status of the nursing child was also monitored. No signals on a negative effect on health of the unborn/newborn children after application of hypertonic saline nasal spray to the patients were observed.
Word
The nasal mucous membrane reacts in a comparable manner on diverse stimuli such as infection, allergy, or other trigger factors with inflammation, edema, and the product of aqueous or gummy hypersecretions. Various clinical symptoms result including impairment of nasal breathing, a runny nose, and sneezing attacks that are ordinarily observed in dissimilar disease entities [3, 4]. Even though many of these diseases, in particular acute viral rhinosinusitis, are self-limiting, patients regularly seek medical aid from doctors and pharmacists in order to relieve their complaints. α-Sympathomimetics are most frequently applied in gild to decrease congestion and thereby to restore free nasal breathing. Topical decongestion of inferior and middle turbinates and infundibular mucosa was demonstrated; clinical benefits across decongestion of these inner structures of the nose, such as sinus and Eustachian tube ventilation and drainage, remain to be demonstrated [eleven, 12]. Furthermore, vasoconstriction induced by nasal decongestants may exist followed by rebound congestion and long-lasting alterations of the nasal mucosa [xiii, xiv]; therefore, these drugs should not exist used for longer than ane week, and special populations such equally significant and chest-feeding women should use α-sympathomimetics only after conscientious risk-benefit-cess [xv].
Hypertonic saline nasal sprays might therefore constitute alternative or at least adjunct treatments to the use of pharmacologically acting decongestants. Beyond the decongesting effect that is accomplished through the osmotic activeness of the solution, saline solutions are ordinarily used for mechanical cleansing and moistening of the nasal mucosa. Moreover, promotion of mucociliary clearance was described for hypertonic saline solutions [16].
The aim of this trial was to evaluate the efficacy and condom of a hypertonic saline nasal spray on various diseases of nose and paranasal sinuses. Some of the indications for employ of the nasal spray (given in Table ii) might exist considered as uncommon, such as apply in case of hyposmia, or even as rather counterproductive, every bit would be the example for use in rhinitis sicca. Due to cooccurrence of disease states, however, such as dry nose symptoms due to an underlying rhinitis medicamentosa [1], collection of such practise-related information remains important. Established indications for use of saline irrigations such every bit astute and chronic rhinosinusitis as well as allergic rhinitis constitute the chief focus of this study, nonetheless [iv,5,half dozen].
The assessment of various disease states under hypertonic saline treatment furthermore allowed us to tease out a more pronounced effect for "rhinosinusitis acute/chronic" vs. "culling to use of α-sympathomimetics" with regard to parameter "nasal discharge, posterior," which is certainly due to the frequent occurrence of this symptom in patients suffering from rhinosinusitis on the 1 hand, but which also can be attributed to a bettering of the overall clinical presentation of these patients. The clinical sum score expressing combined severity of 12 symptoms decreased significantly between initial and final examination during treatment with hypertonic saline nasal spray. Due to potential self-limitations of clinical symptoms, the observed effects were also evaluated for clinical relevance by the included physicians and patients. For more than half of the documented cases, both patients and physicians reported an overall positive result of the treatment and thus would accept or recommend the hypertonic saline spray again under similar conditions, respectively. Approximately 70% of the patients observed an comeback of nasal animate, several fifty-fifty after a very short period of fourth dimension as 1 3rd of the patients noticed improvement already afterward ii or 5 min later application. To our knowledge, this is a first detailed written report on the onset of the clinical upshot of hypertonic saline nasal spray in routine clinical practice, replicating and extending results of an before trial applying rhinomanometry [17].
Concomitant treatments were allowed during the carry of the study in society to maintain the non-interventional graphic symbol and to evaluate the potential boosted benefit from therapy with hypertonic saline. A clear reduction or fifty-fifty abstention from use of α-sympathomimetics must be highlighted as an of import finding of this trial. In particular, patients for which use of these drugs is unsuitable—such as pregnant and nursing women, people suffering from irritated and dry nasal mucosa, or patients having a history of corruption of decongesting nasal sprays that search for non-pharmacological therapeutic options—may profit from treatment with this unproblematic osmotic principle.
Furthermore, our trial confirms the safety of therapy with hypertonic saline. Only one patient reported nigh the occurrence of epistaxis that was rated as potentially related to the application of the nasal spray, and none out of 11 meaning patients and one patient with a nursing child reported any negative effects. Thus, the 2.vii% saline solution nasal spray application showed an overall practiced hazard–benefit ratio which is in accordance with previous findings [18,19,20,21,22]. Male patients were underrepresented in this trial, and this was as well observed in a like report investigating daily hypertonic saline nasal irrigation among patients with sinusitis [23]. Some of the saline applied will be ingested by the patients, which should be considered in populations that should limit their salt consume. Due to the overall low volume applied with the tested nasal spray, this amount tin be neglected, however.
Obviously, the observed results must be reflected confronting the self-limiting course of symptoms for which nasal sprays are used and the uncontrolled report design. The employ of both patient and dr. assessments, in the biometric calculation and estimation of the clinical do good, compensates this drawback in design to a sure extent. In conclusion, the present findings replicate clinical data from controlled studies on illustrating the overall safety and efficacy of diverse nasal hypertonic saline applications [19, 24,25,26,27,28,29].
References
-
Hildenbrand T, Weber RK, Brehmer D. Rhinitis sicca, dry nose and atrophic rhinitis: a review of the literature. Eur Curvation Otorhinolaryngol. 2011;268(1):17–26.
-
Miwa Thousand, Nakajima Northward, Matsunaga M, Watanabe K. Measurement of water loss in human nasal mucosa. Am J Rhinol. 2006;20(five):453–5.
-
Fokkens W, Lund V, Mullol J, Group obotEPPoRaNP. European position paper on rhinosinusitis and nasal polyps. Rhinology. 2007;20(Suppl):1–136.
-
Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012;50(1):i–12. https://doi.org/10.4193/Rhino50E2.
-
Head Thousand, Snidvongs K, Glew Southward, Scadding One thousand, Schilder AG, Philpott C, et al. Saline irrigation for allergic rhinitis. Cochrane Database Syst Rev. 2018;six:Cd012597. https://doi.org/10.1002/14651858.CD012597.pub2.
-
Chong LY, Caput K, Hopkins C, Philpott C, Glew South, Scadding G, et al. Saline irrigation for chronic rhinosinusitis. Cochrane Database Syst Rev. 2016;four:Cd011995. https://doi.org/10.1002/14651858.CD011995.pub2.
-
Brown C, Graham Due south. Nasal irrigations: good or bad? Curr Opin Otolaryngol Head Neck Surg. 2004;12(1):9–13.
-
Principi N, Esposito S. Nasal irrigation: an imprecisely defined medical procedure. Int J Environ Res Public Health. 2017;14(5).
-
Baraniuk J, Ali K, Yuta A, Fang Due south, Naranch K. Hypertonic saline nasal provocation stimulates nociceptive fretfulness, substance P release, and glandular Mucous exocytosis in normal humans. Am J Respir Crit Intendance Med. 1999;160(2):655–62.
-
Insight-Wellness. Over-the-counter sales information (Pharmacies, Germany). Apo-Channel 2013–2018
-
Stringer S, Mancuso A, Avino A. Result of a topical vasoconstrictor on computed tomography of paranasal sinus disease. Laryngoscope. 1993;103(1 Pt i):six–9.
-
Benammar-Englmaier One thousand, Hallermeier J, Englmaier B. Alphamimetische Wirkungen an der Nasenschleimhaut im MR-Tomogramm. Digit Bilddiagn. 1990;10(46–50)
-
Snidvongs K, Thanaviratananich S. Update on intranasal medications in rhinosinusitis. Curr Allergy Asthma Rep. 2017;17(7):017–0720.
-
Ramey JT, Bailen East, Lockey RF. Rhinitis medicamentosa. J Investig Allergol Clin Immunol. 2006;xvi(3):148–55.
-
Mazzotta P, Loebstein R, Koren K. Treating allergic rhinitis in pregnancy. Safety considerations. Drug Safety. 1999;20(iv):361–75.
-
Homer J, Dowley A, Condon Fifty, El-Jassar P, Sood S. The effect of hypertonicity on nasal mucocilliary clearance. Clin Otolaryngol Allied Sci. 2000;25(6):558–60.
-
Michel O, Dressler A. Hypertonic (3%) vs. isotonic alkali nosespray—a controlled study. Laryngorhinootologie. 2011;90(4):206–x.
-
Chirico Thousand, Quartarone G, Mallefet P. Nasal congestion in infants and children: a literature review on efficacy and safety of non-pharmacological treatments. Minerva Pediatr. 2014;66(6):549–57.
-
Garavello Due west, Somigliana E, Acaia B, Gaini 50, Pignataro L, Gaini R. Nasal lavage in meaning women with seasonal allergic rhinitis: a randomized written report. Int Curvation Allergy Immunol. 2010;151(2):137–41.
-
Baraniuk J, Petrie One thousand, Le U, Tai C, Park Y, Yuta A, et al. Neuropathology in rhinosinusitis. Am J Respir Crit Care Med. 2005;171(1):5–11.
-
Baraniuk JN, Ali M, Naranch K. Hypertonic saline nasal provocation and audio-visual rhinometry. Clin Exp Allergy. 2002;32(four):543–fifty.
-
Lenoir J, Bachert C, Remon JP, Adriaens E. The slug mucosal irritation (SMI) assay: a tool for the evaluation of nasal discomfort. Toxicol In Vitro. 2013;27(6):1954–61. https://doi.org/ten.1016/j.tiv.2013.06.018.
-
Rabago D, Zgierska A, Mundt M, Barrett B, Bobula J, Maberry R. Efficacy of daily hypertonic saline nasal irrigation among patients with sinusitis: a randomized controlled trial. J Fam Pract. 2002;51(12):1049–55.
-
Tulupov D, Karpova E, Voropaeva E. A novel view of prophylaxis and treatment of chronic adenoiditis in children. Vestn Otorinolaringol. 2011;one(66.69)
-
Rapiejko P, Jurkiewicz D. The apply of hypertonic sea-h2o solution in patients after surgery of the nose and paranasal sinuses. Otolaryngol Pol. 2010;64(ane):20–30.
-
Friedman M, Vidyasagar R, Joseph Due north. A randomized, prospective, double-bullheaded written report on the efficacy of dead body of water common salt nasal irrigations. Laryngoscope. 2006;116(6):878–82.
-
Garavello W, Di Berardino F, Romagnoli M, Sambataro G, Gaini R. Nasal rinsing with hypertonic solution: an adjunctive treatment for pediatric seasonal allergic rhinoconjunctivitis. Int Arch Allergy Immunol. 2005;137(four):310–4.
-
Rabago D, Pasic T, Zgierska A, Mundt M, Barrett B, Macberry R. The efficacy of hypertonic saline nasal irrigation for chronic sinonasal symptoms. Otolaryngol Head Neck Surg. 2005;133(1):3–eight.
-
Wabnitz D, Wormald P. A blinded, randomized, controlled study on the effect of buffered 0.9% and 3% sodium chloride intranasal sprays on ciliary beat out frequency. Laryngoscope. 2005;115(5):803–five.
Writer information
Affiliations
Corresponding author
Ethics declarations
The trial was performed co-ordinate to the High german Medical Device Deed and the Declaration of Helsinki, was registered in the German Clinical Trial Register (DRKS-ID: DRKS00010825), and was approved by the Institutional Review Board of the Freiburg Ethics Committee International (Code: 016/1245).
Disharmonize of Interest
The trial was funded by URSAPHARM Arzneimittel GmbH. Peter Meiser is employed at URSAPHARM Arzneimittel GmbH. The authors take declared that in that location is no further conflict of interest.
Research Involving Human Participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable upstanding standards.
Informed Consent
Informed consent was obtained from all private participants included in the written report.
Additional data
Publisher'due south Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This commodity is function of the Topical Collection on Medicine
Rights and permissions
Open Access This article is distributed under the terms of the Artistic Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/four.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give advisable credit to the original author(south) and the source, provide a link to the Artistic Commons license, and signal if changes were made.
Reprints and Permissions
Near this article
Cite this article
Bergmann, C., Müller, K., Thieme, U. et al. Real-World Information on the Use of Hypertonic Saline Nasal Spray in ENT Practice. SN Compr. Clin. Med. 1, 354–361 (2019). https://doi.org/x.1007/s42399-019-0050-y
-
Accepted:
-
Published:
-
Issue Date:
-
DOI : https://doi.org/10.1007/s42399-019-0050-y
Keywords
- Hypertonic saline
- Nasal spray
- Rhinitis
- Rhinosinusitis
- Decongestion
- Pregnancy
Source: https://link.springer.com/article/10.1007/s42399-019-0050-y
0 Response to "Can Concentrated Saline Solution Be Bad for a Baby"
Post a Comment